Female Anatomical Reasons for infertility
Infertility is a serious and heartbreaking issue for many around the globe. About 48.5 million couples experience infertility worldwide. In the United States, nearly 1 in 7 couples experience infertility, which means they have been unable to conceive after at least a year of frequent, unprotected intercourse. Although society often first looks to the woman to troubleshoot infertility, it’s also important to look at the male partner. In couples struggling with infertility in developed countries, it’s estimated that 37% of the couples had infertility issues attributed to the female only, 8% of couples had infertility causes attributed to the male only, and 35% of couples had infertility causes attributed to both the female and male (1).
In this series, we will cover a multitude of reasons for infertility and what can be done about them. In this first article, we will talk solely about female anatomical reasons for infertility.
Signs and Symptoms of Female Infertility
There are a few signs that show that infertility may be a potential issue, aside from not being able to conceive a child. Signs and symptoms of female infertility may include:
irregular periods
painful or heavy periods
no periods
hormone fluctuation symptoms (e.g., facial hair growth, reduced libido, skin issues, weight gain)
pain during intercourse
Anatomical Issues Causing Female Infertility
There are a number of anatomical issues that cause infertility among females. Anatomical issues account for about 40% of the reasons women in developed countries are infertile. When addressing infertility, anatomical reasons should always be explored and ruled out or addressed first. We list and describe a few briefly below.
Tubal abnormalities (tubal factor infertility)
Tubal abnormalities refer to a blockage or adhesion in the fallopian tubes. Fallopian tubes can be either completely blocked or just have one blocked tube or scarring that narrows the tube (2). Having clear fallopian tubes is very important for positive pregnancy outcomes, because they facilitate the transport of the egg cells from the ovary to the uterus each month. Clear fallopian tubes also allow sperm to pass through, and if fertilization occurs, the fallopian tubes will transport the fertilized egg to the uterus for implantation. If both tubes are completely blocked, it’s impossible to get pregnant. If tubes are partially blocked pregnancy may be possible, but an ectopic pregnancy may occur.
If both tubes are completely blocked, it’s impossible to get pregnant. If tubes are partially blocked, pregnancy may be possible, but an ectopic pregnancy may occur.
Causes for tubal abnormalities:
Between 25-30% of women who have an infertility evaluation have tubal abnormalities. The biggest cause for these abnormalities is having pelvic inflammatory disease (PID), as PID can travel from the cervix to the uterus to the tubes. A previous ectopic pregnancy may also cause tubal abnormalities. Additionally, infections, such as chlamydia and gonorrhea, can cause tube damage, as well as other diseases like endometriosis and tuberculosis. Abdominal surgery or a burst appendix may also cause tubal factor infection and subsequently, tubal factor infertility (2).
Between 25-30% of women who have an infertility evaluation have tubal abnormalities
Treatment for tubal abnormalities:
If a fallopian tube is blocked by scar tissue or adhesions, laparoscopic surgery may be an option.
If the blockage is larger, more significant surgery to repair the tubes may help. It’s possible to remove the damaged part of the tube and connect the two healthy parts to restore function.
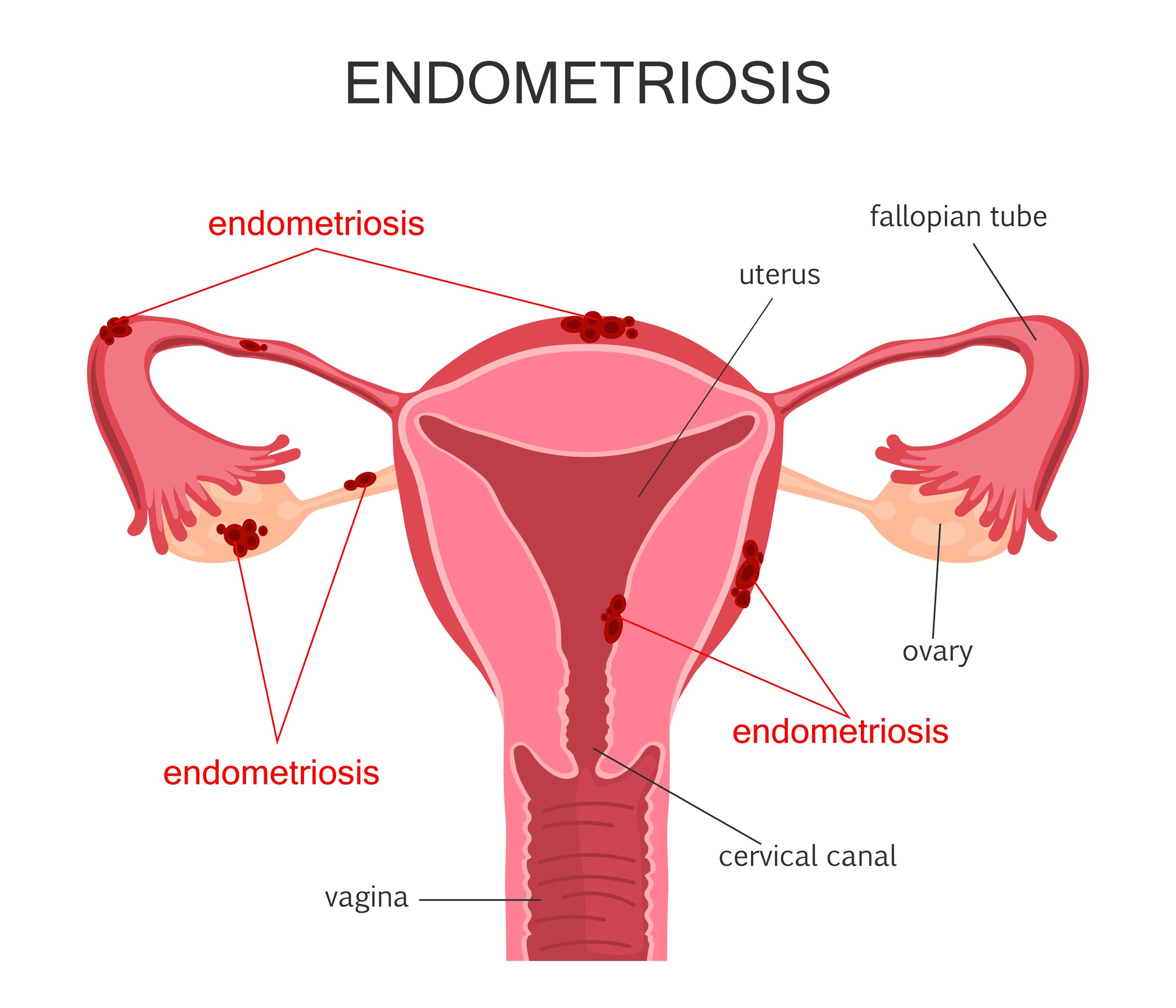
Endometriosis
Endometriosis occurs when the tissue that normally lines the uterus grows to places outside of the uterus, including the ovaries, fallopian tubes, or the intestines. Endometriosis is a very common condition that causes both pain and infertility, though 20-25% of women who have endometriosis are asymptomatic (4).
6-10% of women have endometriosis, and 30-50% of women who have endometriosis are infertile. Among women who have been diagnosed as infertile, 25-50% of these women have endometriosis (3).
It is thought that a variety of factors are at play, including immunological, genetic, and environmental factors (4).
Causes for endometriosis (3,4):
Retrograde menstruation- This is when menstrual blood that contains endometrial cells goes back into the fallopian tubes and into the pelvic cavity rather than leaving the body. The endometrial cells then stick to the pelvic walls or different surfaces of the pelvic cavity, and they continue to thicken there.
Transformation of peritoneal cells (“induction theory”)- Some experts theorize that peritoneal cells (cells that line the inner side of the abdomen) transform into endometrial-like cells due to hormones or immune factors.
Embryonic cell transformation- Estrogen or other hormones may transform embryonic cells into endometrial-like cells implants during puberty.
Surgical scar implantation- Post-surgery, endometrial cells may attach to a surgical incision.
Endometrial cell transport- Blood vessels or tissue fluid may transplant endometrial cells to different parts of the body.
Immune system disorder- A dysregulated immune system may not allow the body to recognize and destroy endometrial-like tissue that is growing outside the uterus.
Hormone imbalance of estrogen and progesterone- While we don’t know if a hormone imbalance causes endometriosis to start, we do know that if you have endometriosis and have endometrial cells growing outside of the uterine cavity, progesterone and estrogen signaling are disrupted. This results in low progesterone and estrogen dominance, which causes inflammation. This hormone imbalance may also result in increased pelvic pain and decreased chance of successful embryo implantation. Endometrial cells thrive on estrogen and additionally, make their own estrogen. High estrogen levels are a marker of endometriosis.
Symptoms for endometriosis may include:
Painful periods
Painful intercourse
Pain with urination or bowel movements
Excessive bleeding (heavy periods, bleeding in between periods, or both)
Fatigue, diarrhea, constipation, nausea, or bloating, especially during menstruation
Many women who have endometriosis also have irritable bowel syndrome (IBS) and many food intolerances, such as gluten, soy, caffeine, legumes, and dairy. As noted, digestive issues often become worse during menstruation.
Treatment for endometriosis:
Treatment may include taking hormones or surgery, including both electrosurgery and laparoscopic surgery. Though taking hormones may reduce symptoms, there is not as much evidence to show that it improves pregnancy outcomes. Rather, surgical removal of endometriotic implants appears to have better chances of a successful pregnancy. If a pregnancy does not occur after surgery, in vitro fertilization and embryo transfer (IVF-ET) has been a successful follow up to surgery for many women (6).
Though there are currently no research studies to make a conclusion, diet may also play a role in endometriosis. Increasing omega 3s, vitamin D, and antioxidants, while avoiding inflammatory foods like gluten and trans fats may reduce pelvic pain and could potentially contribute to a positive pregnancy outcome, particularly in combination with surgery (7).
At our office, we check food sensitivity panels as well as Omega-3 and Omega-6 levels. Avoiding inflammatory foods can do wonders to manage the condition, and omega 3 fatty acids will reduce inflammation in the body. Research has shown that high ratios of omega-6 fatty acids to omega-3 fatty acids are markers for disease severity of endometriosis (8). This is also why taking omega-3 fatty acids will help reduce menstrual cramping.
Uterine myomas/fibroids
Uterine myomas are better known as fibroids, and these can distort the uterine cavity, reduce surface area for implantation, and cause inflammation in the body. (It’s important to note that you can also have endometrial fibroids.) Fibroids affect 20-50% of women of reproductive age. Symptoms can include heavy periods, prolonged periods, and pelvic pain, though in some cases, there are no symptoms. Uterine myomas or fibroids can affect fertility by distorting the cervix and uterus, negatively impacting egg movement, or blocking the fallopian tubes (9).Though it’s hard to pinpoint the exact cause of fibroids, the medical community believes that hormones, growth factors (e.g., insulin growth factor), or genetic changes within fibroids may play a role (10).
Risk factors for uterine fibroids can include (11, 12):
Lack of physical activity
Obesity
Diet
Hormones
Age (older women more at risk)
Race (African Americans more at risk)
Family history of uterine fibroids
High blood pressure
Vitamin D deficiency
No history of pregnancy
Consumption of food additives
Endocrine disrupting chemicals
Treatment for uterine fibroids:
Myomectomy - This is a surgical procedure to remove fibroids. You may need to wait 3 months before trying to conceive again and it may increase the chance of cesarean delivery.
Myolysis - A myolysis uses a laser, radio-frequency energy beam, or electric current to shrink the blood vessels that feed the fibroids.
Hormonal birth control pills- This may ease symptoms, but may also increase the size of fibroids. It also won’t allow you to become pregnant while on the pill.
Intrauterine device (IUD) - This method may also ease symptoms, but will not reduce fibroids and also prevent pregnancy from occurring.
Gonadotropin-releasing hormone (Gn-RH) agonists - This method will shrink fibroids, but because it blocks hormones that allow for ovulation and menstruation, you will not be able to conceive while on the medication.
Pelvic adhesions
Pelvic adhesions are when scar tissues cause internal organs to stick to one another, such as the uterus, ovaries, fallopian tubes, bladder, and intestines. They could cause different organs to stick to each other, such as uterus binding to the ovaries. They could also cause bonding within the organ, such as one part of the uterine wall binding to the opposite side (13).
Causes of pelvic adhesions - Oftentimes, pelvic adhesions are caused by pelvic surgery or infection. PID (pelvic inflammatory disease) often leads to adhesions in the fallopian tubes. Endometriosis, in severe cases, may also lead to pelvic adhesions (13).
Treatment for pelvic adhesions - As with many of the anatomical issues for infertility, surgery is the only appropriate treatment for pelvic adhesions to remove the physical issue. Laparoscopic surgery and laparotomy are two commonly used surgery procedures for pelvic adhesions.
Congenital uterine anomalies
During development in utero, a female baby’s uterus forms as two separate halves that then fuse together when she is born. However, sometimes (estimated at less than 5% of women) the uterus can form abnormally, which is when congenital uterine anomalies occur. Anomalies may include the two halves of the uterus remaining separate (didelphys), only one half of the uterus developing (unicornuate), a normal uterine surface with a slight indentation into the endometrial cavity (arcuate), an indented uterine surface and two endometrial cavities (bicornuate), or a normal uterine surface with two endometrial cavities (septate) (14). Though less than 5% of women are affected by congenital uterine anomalies, they have been noticed in up to 25% of women who have miscarriages or premature births and can also increase the risk of infertility (15).
Treatment for congenital uterine anomalies - Most women with congenital uterine anomalies can have the problem remediated through minimally invasive surgery, such as laparoscopy or hysteroscopy. In the case of a unicornuate uterus, the obstructed part of the uterus may be removed if the other half is functioning.
Though many of the treatments for female anatomical infertility causes include surgery, it’s also extremely important to address any hormone imbalances or inflammatory issues that are contributing to the above infertility causes.
Please contact our office so we can help. Also look out for our next article, which addresses male anatomical infertility causes.
Works cited:
https://apps.who.int/iris/bitstream/handle/10665/38679/WHO_TRS_820_eng.pdf?sequence=1&isAllowed=y
Kharrazian, D. (2020). Infertility, prenatal care, and maternal health clinical strategies and treatment applications [PowerPoint presentation]. Kharrazian Institute.
https://www.verywellhealth.com/endometriosis-diet-pregnancy-4134664
https://www.mayoclinic.org/diseases-conditions/uterine-fibroids/symptoms-causes/syc-20354288
https://www.nichd.nih.gov/health/topics/uterine/conditioninfo/people-affected