Why Ditching Gluten and Dairy May Help Autoimmune Thyroid Disease
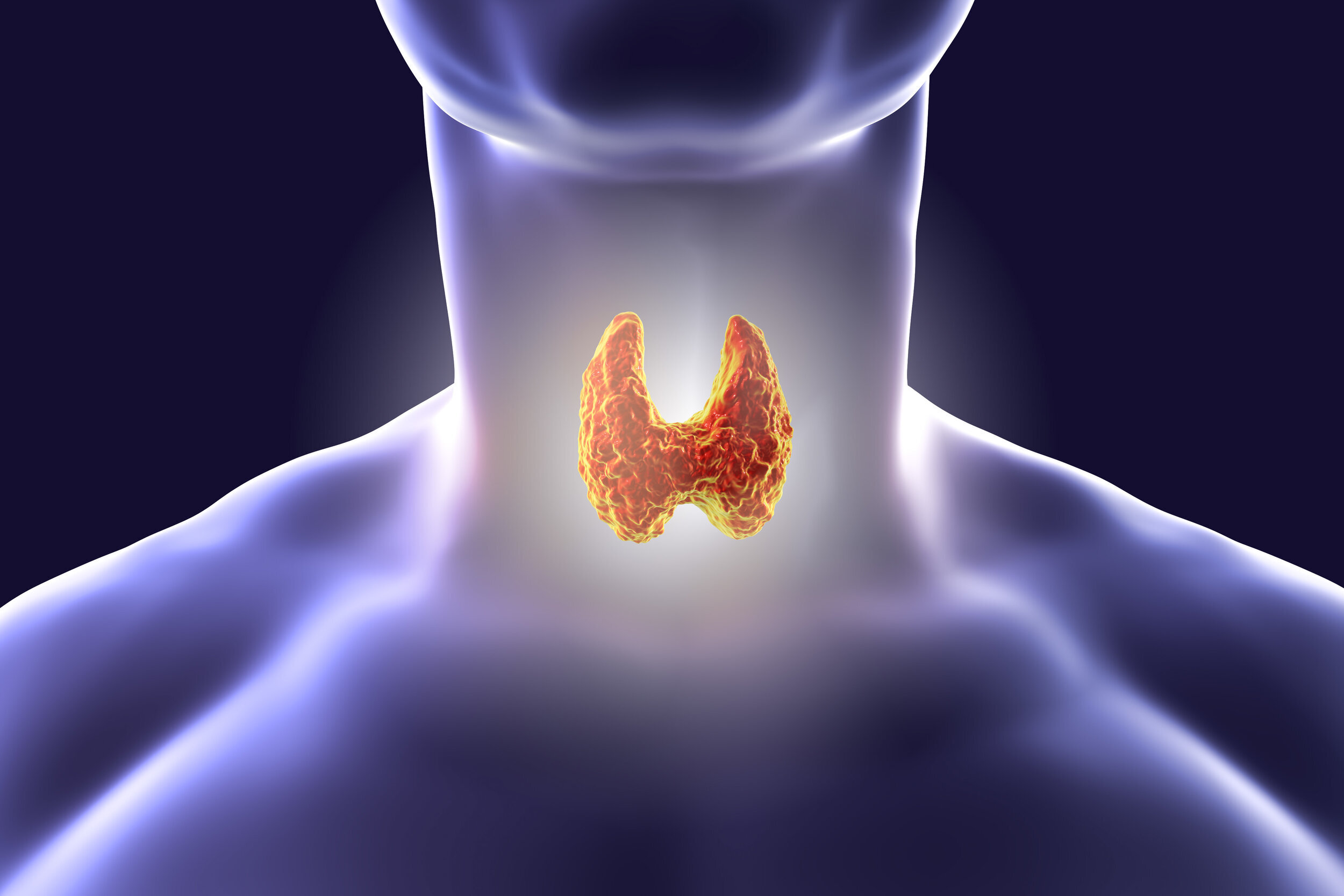
The thyroid is a butterfly-shaped gland in the lower front of the neck that produces hormones which regulate many body functions, including metabolism, heart function, digestion, muscle control, brain development, mood regulation, and bone maintenance. It is vital to your overall function and wellness. That being said, there is a growing increase in those who are dealing with a thyroid condition, including autoimmune thyroid disease (AITD), such as Hashimoto’s thyroiditis (autoimmune hypothyroidism) or Graves’ disease (autoimmune hyperthyroidism).
AITD is an autoimmune condition in which the thyroid is destroyed by the immune system. In this condition, the immune system pecks away at the thyroid. A thyroid should have homogenous edges, which are round and smooth on this butterfly-shaped gland. In an inflamed state with AITD, the gland will often be enlarged. If the AITD is not handled properly, over time, it will result in a smaller than normal gland size, indicating atrophy. This process results in decreased thyroid hormone output, which results in worsening of symptoms. Anything that enhances the immune response against the thyroid will increase the thyroid atrophy and destroy the thyroid faster.
Thyroid under attack from antibodies
To understand autoimmunity of the thyroid, it’s also important to understand acquired immunity. Acquired immunity is the immune system’s adaptive response to a pathogen, and it is the rationale behind the creation of vaccines. When the immune system encounters a pathogen, highly specialized cells form a response and remember the pathogen by identifying its antigen, so when it is encountered again, the response is enhanced to destroy the pathogen. In the acquired immune system, pathogen-specific receptors are acquired throughout the life of the organism in order to flag and destroy invading pathogens. However, in this process, the immune system may have a misdirected response in which it responds in this aggressive manner to its own tissue.
One of the mechanisms that can lead to this misdirected response is cellular mimicry, which is when the immune system flags both a pathogen and an innocent tissue in the body as one in the same and tries to destroy both. This is the case in AITD. Though researchers are still working to find out why some people may be susceptible to autoimmune conditions than others, we know that risk factors may include:
Genetics
Exposure to certain environmental toxins
Having a leaky gut
Previous infections
Age (young to middle-aged)
Gender (women account for 80% of those with autoimmune conditions)
Ethnicity (African American, Latino, and American Indian are more likely to develop autoimmune conditions than Caucasians)
You may have heard that if you deal with AITD, it is wise to keep gluten, and perhaps even dairy, out of your diet. This can be a hard pill to swallow for those of us who consider bread, milk, and cheese staples in our diets. In this article, we discuss why the consumption of gluten and dairy can be problematic for those with AITD and if gluten and dairy are inflammatory in general. Additionally, we discuss other foods that may be problematic for the thyroid.
Gluten and AITD
Gluten is a protein in various grains, including wheat, barley, and rye. Gluten contains a protein called gliadin, and the molecular structure of gliadin is very similar to transglutaminase - an enzyme that present throughout the body to make chemical bonds. This enzyme is abundant both in the intestines and in the thyroid. If you have AITD, your body is producing antibodies that attack transglutaminase in the thyroid. (1,2)
When you eat gluten, and the intestines are exposed to gliadin, the gliadin leads to zonulin upregulation, which loosens the tight junctions of the intestines and increases intestinal permeability. This intestinal permeability occurs in ALL persons, regardless of if a person has a gluten sensitivity or not (3). Because intestinal permeability increases, the gliadin is then able to make its way beyond the gut barrier and into the bloodstream.
Because of gliadin’s similar molecular structure to transglutaminase (4), the body may tag it in the bloodstream as a foreign invader that should also be attacked. This may then prompt your body in its heightened state to attack both gliadin and transglutaminase, the enzyme prolific in the thyroid, because of their structural similarities. In other words, whenever gliadin is in the bloodstream, the body may raise an immune response to gliadin and also attack the thyroid.
Research has shown that eliminating gluten in patients with AITD can significantly reduce thyroid antibody titers (5). While we don’t know the exact percentages, research has also shown that there is a correlation between AITD and celiac disease (CD), which is an autoimmune condition that causes intestinal damage with the consumption of gluten. The occurrence of CD is significantly increased in those with AITD. It is important to screen AITD patients for CD and screen patients with CD for AITD (6,7). It’s estimated that in those with AITD, 2-5% also have CD (8). A diagnosis of CD is most likely confirmed with genetic markers (HLA DQ2 or HLA DQ8) along with a biopsy. For a thyroid disease diagnosis, see here.
Gluten and Inflammation
We are learning that one does not have to have CD in order to suffer from adverse effects of gluten. There is a lot of research documenting the inflammatory nature of gluten, including its ability to increase intestinal permeability and induce inflammatory responses, both in patients with CD and those without. Increased intestinal permeability can then lead to a number of chronic health conditions, including rheumatoid arthritis, multiple sclerosis, inflammatory bowel disease, asthma, chronic fatigue syndrome, and depression (9). As noted previously, the intestinal permeability, or leaky gut, caused by gluten can also lead to AITD. When gliadin is able to pass through the intestinal wall, the body has the potential to flag it as an invader and then create antibodies for both gliadin and the thyroid because of their similar protein structure. Additionally, with increased specificity and sensitivity in stool testing, we are learning that far more people are gluten sensitive than we once believed (10).
Gluten sensitivity symptoms may include
bloating
diarrhea
constipation
abdominal pain
anemia
fatigue
brain fog
headaches
eczema and other rashes
depression and/or anxiety (11)
Many of these symptoms correlate with a thyroid condition as well.
For those with CD or AITD (or anyone who suspects a non-celiac gluten sensitivity), it’s very important to be completely gluten free, as the effects of gluten consumption last up to six months. While those with a non-celiac gluten sensitivity or CD may experience unpleasant digestive symptoms upon consuming gluten, their thyroid health may also suffer (12).
Dairy and AITD
Another food that may be worth restricting in those with AITD is dairy. In patients with AITD, lactose intolerance may also be an issue. In one study, patients with Hashimoto’s who also tested positive for lactose intolerance significantly improved their TSH (thyroid stimulating hormone) levels after restricting lactose for eight weeks (13).
Casein, the protein found in dairy, is very structurally similar to gliadin, the protein in gluten. When your body reacts to gluten, there’s a good chance it can also react to dairy because of this protein. If the body sees gliadin as a pathogen, there is a good chance it might recognize casein as a pathogen as well, due to their similar structures. In this case, it may then raise the same immune response for casein as it does for gliadin. In one small study with patients who had CD, about 50% of these patients had a similar inflammatory response to cow’s milk as they did to gluten (14).
Dairy and Inflammation
Dairy also tends to be on the inflammatory side for many, primarily due to the sugar (lactose) and proteins (casein and whey) found in it. Those with lactose intolerance have the inability to digest lactose, and it’s estimated that as much as 65% of the human population is lactose intolerant (15).
Additionally, many struggle with digesting the casein in milk, moreso, the A1-beta casein milk, which has a similar protein structure to gliadin. In animal studies, digestion of casein, specifically A1-beta casein found in conventional dairy, can increase gastrointestinal time as well as the production of inflammatory markers when compared to A2-beta casein milk. In humans, participants who consumed A2 milk compared to those who consumed A1 milk had statistically significantly higher Bristol stool values as well as less abdominal pain (16).
In another study, A1-beta casein milk was associated with increased gastrointestinal inflammation, increased digestive discomfort, delayed transit, and decreased cognitive speed and accuracy, while A2 beta- casein did not produce these symptoms (17). However, when making dietary changes, it is wise to eliminate all casein from the diet first in case you are extremely casein sensitive. Then you might wish to try A2 milk from Jersey cows, goats, or sheep to see if you are able to tolerate it.
Clinical Results of Going Gluten and Dairy Free
Clinically, it is easy to see the benefits of going gluten and dairy free when you have a thyroid condition. In a clinical survey of 2,232 people who had Hashimoto’s, 88% of those who went gluten free felt better, 3.2% felt worse, and 33% reduced their thyroid antibodies. In the same sample, in those who went dairy free, 79% felt better, 1.5% felt worse, and 20% reduced their thyroid antibodies (18).
In another study of 38 patients who had both Hashimoto’s and lactose intolerance, after eliminating dairy, 75% of these patients decreased their thyroid stimulating hormone levels (19).
Considering how common the digestion struggles of gluten and dairy are, it’s no surprise that eliminating them could help with AITD.
Other Cross Reactive Foods
You may find that you are still experiencing gluten sensitivity symptoms after going gluten, and even dairy free. Do you remember how dairy can present an issue because its protein is similar to gliadin- the protein in gluten? There are a few other foods that can also produce a cross reaction. Because their protein structures are similar to gluten (and the thyroid enzyme, transglutaminase), the body flags them as invaders and builds an immune response, increasing your inflammation and unpleasant symptoms.
These cross reactive foods includes:
Yeast
Oats
Corn
Millet
Instant coffee (and even ground coffee are often contaminated by gluten- grind your own coffee beans)
Rice (20)
For a more complete list of cross reactive foods, see the chart below.
If you are are gluten free and find that you are still experiencing the same symptoms from consuming gluten, try eliminating these foods as well.
If you have autoimmune thyroid disease, we feel it is highly important to try eliminating gluten and dairy from your diet. Research, along with our own clinical experience, has proven that a gluten free/dairy free lifestyle is an important factor in both maintaining an autoimmune thyroid condition and healing an autoimmune thyroid condition. Though cutting these foods may seem overwhelming at the beginning, we know you will find that a nutrient-dense diet without them will allow you to feel more like your best self. Please contact our office for more information. We would love to help you in this journey!