SIBO: A common digestive disorder that is often missed
What is SIBO?
Small intestine bacterial overgrowth (SIBO) is an overgrowth of the bacterial population in the small intestine that often goes undiagnosed. Typically, the types of bacteria found in SIBO are foreign to the small intestine environment. Symptoms of this disorder can range from mild to severe, depending on how much dysfunction has developed (1).
Basics of Digestion and SIBO:
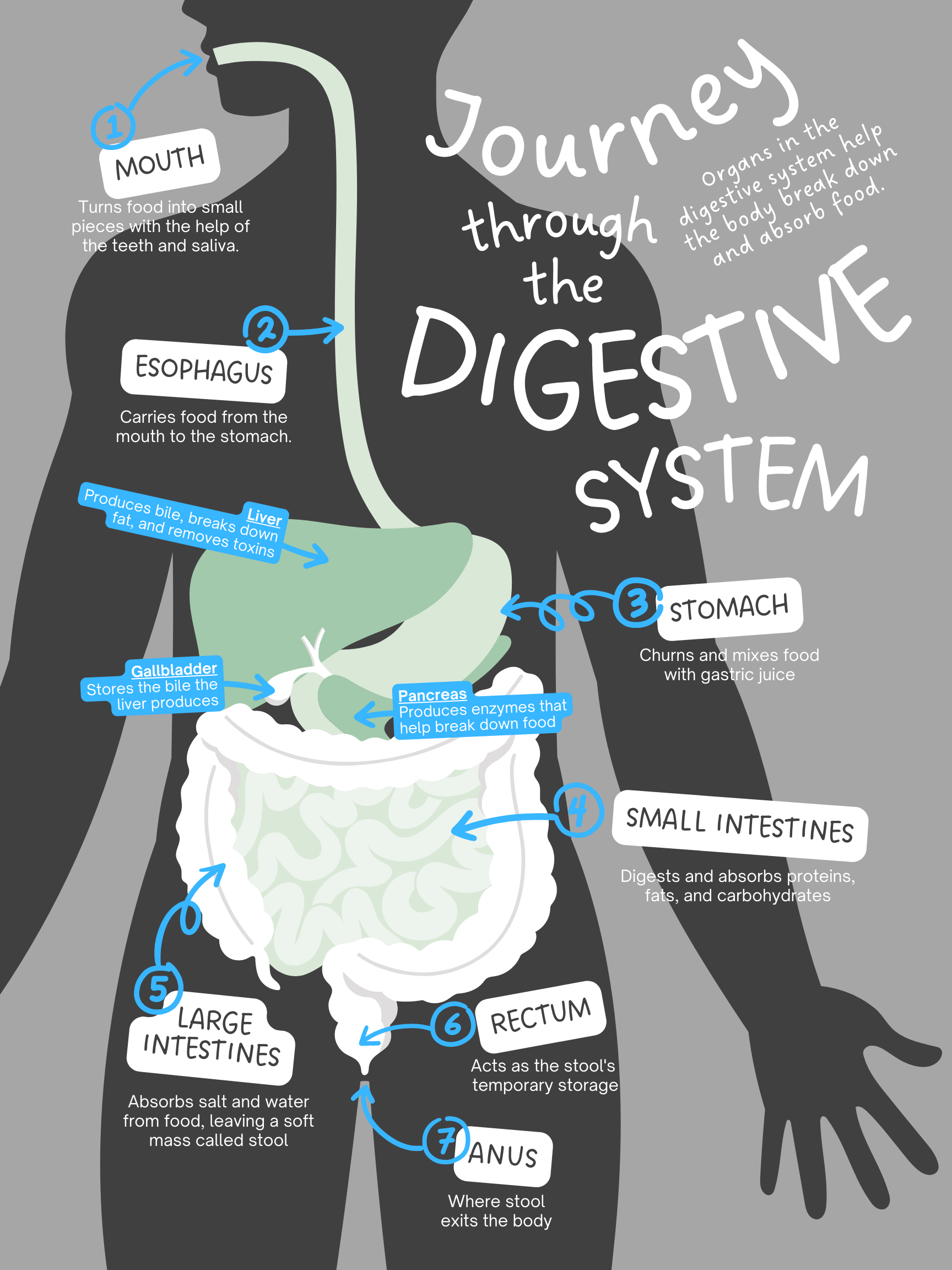
The digestive tract, also known as the gastrointestinal tract (GI), digests food by breaking it down and absorbing nutrients. The mouth, pharynx, esophagus, stomach, and intestines are all part of the GI tract. Smooth muscles in these regions move food through the GI tract while enzymes break the food down. The GI tract is also made up of the salivary glands, the liver, the pancreas, and the gallbladder, which supply digestive juices. These digestive juices and stomach acids, also known as gastric juices and gastric acids, are highly acidic and are produced to break the food down in the stomach. Signals from the autonomic nervous system and hormones stimulate this gastric acid production (2). Hydrochloric acid, also a stomach juice, helps in the breakdown process and also kills pathogens. Digestive enzymes split proteins, carbohydrates and fats to aid in assimilation, the absorption and digestion of food and nutrients. (3). Enzymes also help to break down fat and carbohydrates.
After food is digested in the stomach, it passes through the small intestine where nutrients from the food are absorbed. The leftover remnants are then pushed through into the large intestine, where they are turned into feces as water extraction takes place. Under normal conditions, the large intestine is the primary carrier of bacteria and microbes.
When this process isn’t functioning correctly, bacteria can build up in the small intestine. Some causes of dysfunction include decreased digestive acid and juices, decreased speed of processing food through the small intestine, or damage in the intestines. Whatever the cause, dysfunction can lead to various symptoms such as abdominal pain, gas and bloating, and diarrhea or constipation. As harmful bacteria overpopulate the gut, they release toxins which damage the mucosa, a membrane that lines and lubricates the GI tract to protect the body from invading pathogens. A damaged mucosa can lead to malabsorption, a condition in which the body isn’t receiving the proper amount of nutrients, and can eventually cause nutrient deficiencies and inflammation (4). Harmful bacteria also inhibit gastric acid secretion by the parietal cells in the stomach. These secretions are needed to keep the bacteria count under control (5). Gastric acid secretion also aids in the absorption of nutrients, kills pathogens, and prevents intestinal infections.
SIBO is a severe form of dysbiosis or “leaky gut”. Dysbiosis occurs when there is a disruption of the epithelial layer which makes up the mucosa. This epithelial layer functions as a barrier and is responsible for secretion as well as absorption. When dysbiosis occurs, this layer becomes permeable, allowing bacteria, chemicals, and toxins to leak out into the bloodstream. This causes inflammation and can contribute to autoimmune issues and neurodegenerative disorders.
A number of factors contribute to dysbiosis. Poor diet, stress, synthetic hormones, acid blockers, infections, and antibiotics which prevent the GI tract from producing the right amount of nutrients and hormones, are some of the most common factors. These factors can influence the flora (microorganisms) of the gut, creating an unhealthy environment in the GI tract where SIBO can take over.
The following symptoms are common indicators of SIBO:
Types of SIBO:
Methane dominant (SIBO-C) Also known as constipation SIBO. When methanogens (methane producing bacteria), such as Methanobrevibacter smithii, overpopulate the small intestine, they take in and thrive on the hydrogen in your gut and produce methane. This slows down transit in the intestines (6).
Hydrogen dominant (SIBO-D) In this type, hydrogen-producing bacteria overgrowth produces an excessive amount of hydrogen gas. This form is known for the symptoms of diarrhea and bloating.
Mixed. A combination of methane and hydrogen dominant SIBO.
Hydrogen sulfide dominant (SIBO-HS) This type of SIBO occurs when Desulffovibrio spp. bacteria produce an abundance of hydrogen sulfide gas, which is toxic to the body.
Small intestine fungal overgrowth (SIFO) Similar to SIBO, small intestinal fungal overgrowth or SIFO, occurs when there is an overgrowth of fungus. SIFO has similar symptoms to that of SIBO. SIFO and SIBO can be seen together, as 20% of SIBO patients are also diagnosed with SIFO (2). Up to 5% of SIBO cases are misdiagnosed as SIBO. Since there is no test for SIFO, finding fungus in stool along with SIBO symptoms can be a good indicator that the patient has SIFO.
Common deficiencies associated with SIBO:
The GI tract has the largest microbial population in the entire body, housing 500 different types of bacteria. In a healthy digestive system, these bacteria aid in the digestion of food. However, when there are too many bacteria or microbes in the GI tract, these bacteria compete for the body’s nutrients, stealing vitamins and preventing homeostasis. Here are some of the deficiencies associated with the overgrowth of bacteria:
Inability to absorb fat soluble vitamins Bile in the stomach enables the extraction of fats from food. SIBO interferes with bile acids, making it difficult to absorb fat soluble vitamins, such as Vitamin A, Vitamin D, Vitamin E, Vitamin K, and essential fatty acids (4).
Exocrine Pancreatic Insufficiency (EPI): In a healthy functioning body, the pancreas digests, absorbs, and metabolizes nutrients with the aid of pancreatic enzymes. With exocrine insufficiency (EPI), the pancreas doesn’t produce enough digestive enzymes (7). This can lead to malabsorption, the result of food not being properly converted into stable energy by the digestive system. In 30-40% of cases of chronic pancreatitis (EPI), SIBO worsens the condition (1), affecting the gut flora, aiding in malabsorption. SIBO interferes with the normal chyme (digestive acids and juices) of the small intestines, motility of the digestive tract, and the amount of proteolytic enzymes which kill off harmful amounts of bacteria in the small intestines. (1)
B12 deficiency: Commonly seen side effects of B12 deficiency include neurological issues, pain, and anemia (a deficiency of red blood cells).
Iron deficiency: With a deficiency of iron, the body becomes anemic, causing fatigue.
Neurological: The vagus nerve is the tenth cranial nerve connecting the brainstem in the neck to the abdomen. It is responsible for regulating the functions of the nervous system, such as the heartbeat and respiration, and the inflammatory system. Blinking and other reflex actions, urination, and the function of the liver and kidneys are also controlled by this nerve. The vagus nerve also sends signals which connect the GI tract to emotional and cognitive functions. Related to SIBO, the vagus nerve also plays a big role in digestion, stimulating the stomach, liver, pancreas, and intestines. It controls contractions in the smooth muscles, secretion in the epithelial glands, and intestinal permeability. When intestinal permeability is affected, leaky gut manifests. This is a digestive condition in which bacteria and toxins are able to leak through the intestinal wall into the body causing inflammation that can lead to autoimmune conditions. When the vagus nerve is not functioning properly due to deficiencies often caused by stress and anxiety, it can also slow down the digestive processes and SIBO can occur, leading to other inflammatory issues like heartburn, IBS, and inflammatory bowel disease (8).
Root issues with SIBO:
Many seemingly healthy patients are diagnosed with SIBO, but it is most commonly found in older individuals, women, and the overweight and obese. SIBO also thrives in those who are immuno-compromised, as well as in those with other GI disorders. People who have food intolerances are also at risk for developing SIBO. Many other factors contribute to the development of SIBO, including the overuse of antibiotics or certain medications, surgery and some of the underlying conditions/diseases listed here:
Hypothyroidism: SIBO is seen in more than half of patients diagnosed with hypothyroidism (9). Hypothyroidism slows down the body’s processes, including digestion. An under-active thyroid does not make enough HCL (hydrochloric acid), one of the main stomach juices which aids in food digestion, and this prevents the body from digesting food properly leading to malabsorption. Hypothyroid patients also experience frequent constipation. This causes the GI tract to become a breeding ground for SIBO since the intestines don’t remove waste and push out bacteria fast enough. (10)
Mold Illness: Exposure to mold can create leaky gut. Mold and mycotoxins harm microflora and can cause inflammation and digestive dysfunction.
Migrating Motor Complex Dysfunction (MMC): The MMC's job is to move undigested food through the small intestine. This is done in three phases of contractions which clean out the stomach and intestines during the fasting period before the next meal. Motolin, a hormone produced by the small intestine and the main hormone regulator of the MMC, is released during these phases (12). When there is a dysfunction in the migrating motor complex, SIBO can interfere with contractions and hormone production by slowing down the motility.
Birth control: Hormonal birth control causes motility issues in digestion through the impact of the gallbladder.
Antibiotics: These medications wipe out both the helpful and harmful bacteria of the gut. This causes a disruption of the microbiome (gut flora) and allows the gut to become a breeding ground for drug-resistant bacteria, making SIBO difficult to treat once it invades.
Opioid drugs: When given to patients after surgery, opioid drugs can slow motility in the GI tract.
H. pylori: Helicobacter pylori is an infection of the stomach or duodenum, the first part of the small intestine. This infection shuts down hydrochloric acid production. Hydrochloric acid (HCL) is a digestive juice that breaks down food and helps in nutrient absorption. When HCL is low, protein isn't broken down correctly and nutrient absorption is decreased. H-pylori also lowers the pH in the gut, making the stomach acid less acidic, allowing for SIBO to take place.
Antacids: Consistent use of acid-reducing drugs inhibits stomach acid function. This can lead to bacterial overgrowth.
Prolonged use of Proton Pump Inhibitors (PPI): PPI drugs reduce the amount of acid produced in the stomach. This prevents the proper absorption of nutrients.
Stress: Stress can cause a decrease in stomach acid production, as well as impairing the migrating motor complex (removal of food from the digestive system).
Food poisoning: Food poisoning is caused by pathogenic bacteria (bacteria unfamiliar to the intestines) that release a toxin which can damage the nerve cells in the small intestines. These nerve cells are the ones that regulate the intestines, damaging the MMC and encouraging development of SIBO.
Endometriosis: This causes abdominal lesions, as well as lesions on the bowel which rearrange the positioning of nearby organs and the intestines (13).
Surgery of damage to the lining of the intestines: Scar bands or adhesions from this surgery can form after abdominal surgery, affecting the intestines.
An obstruction: When an obstruction caused by a piece of anatomy or other material occurs, the obstruction can block the area where extra bacteria need to be released from the body. This can happen after abdominal surgery,
Conditions usually associated with SIBO:
Many diseases and immune conditions weaken the immune system and motility of the GI tract, allowing SIBO to manifest. In patients diagnosed with SIBO, 90% of them have been shown to have chronic pancreatitis and small intestine motility disorders. One third of individuals with diabetes have SIBO. Many SIBO patients have coinciding conditions such as liver cirrhosis at 50-60%, irritable bowel syndrome 30-85%, Celiac 9-55%, Crohn’s 25%, Scleroderma 43-56%, and Cystic fibrosis at 56% (1). Osteoporosis is often seen as a side effect of SIBO.