6 Anatomical Reasons For Male Infertility
Article written by Dr. Abigail Vermeesch BCDHH, CNHP, CHS, BS
Infertility Statistics
In a previous article, we discussed the anatomical causes for female infertility, potential mechanisms behind them, and treatment options. In this article, we will discuss anatomical reasons for male infertility. If you remember from our previous article, it’s estimated that 37% of couples struggling with infertility in developed countries have infertility issues attributed to the female only. However, 8% of these couples had infertility causes attributed to the male only, and 35% of couples had infertility causes attributed to both the female and male. When looking at potential causes of infertility, it’s extremely important to look at the male as well.
Signs of Male infertility:
Oftentimes, there are no major signs or symptoms of male infertility aside from not being able to conceive a child. However, there are times when signs point to infertility. These signs include:
Sexual dysfunction, including low libido, erectile dysfunction, and problems with ejaculation
Lump, pain, or swelling in the testicular area
Frequent respiratory infections
Breast growth (gynecomastia)
Inability to smell
Decreased facial or body hair
anatomical Complications In Male fertility
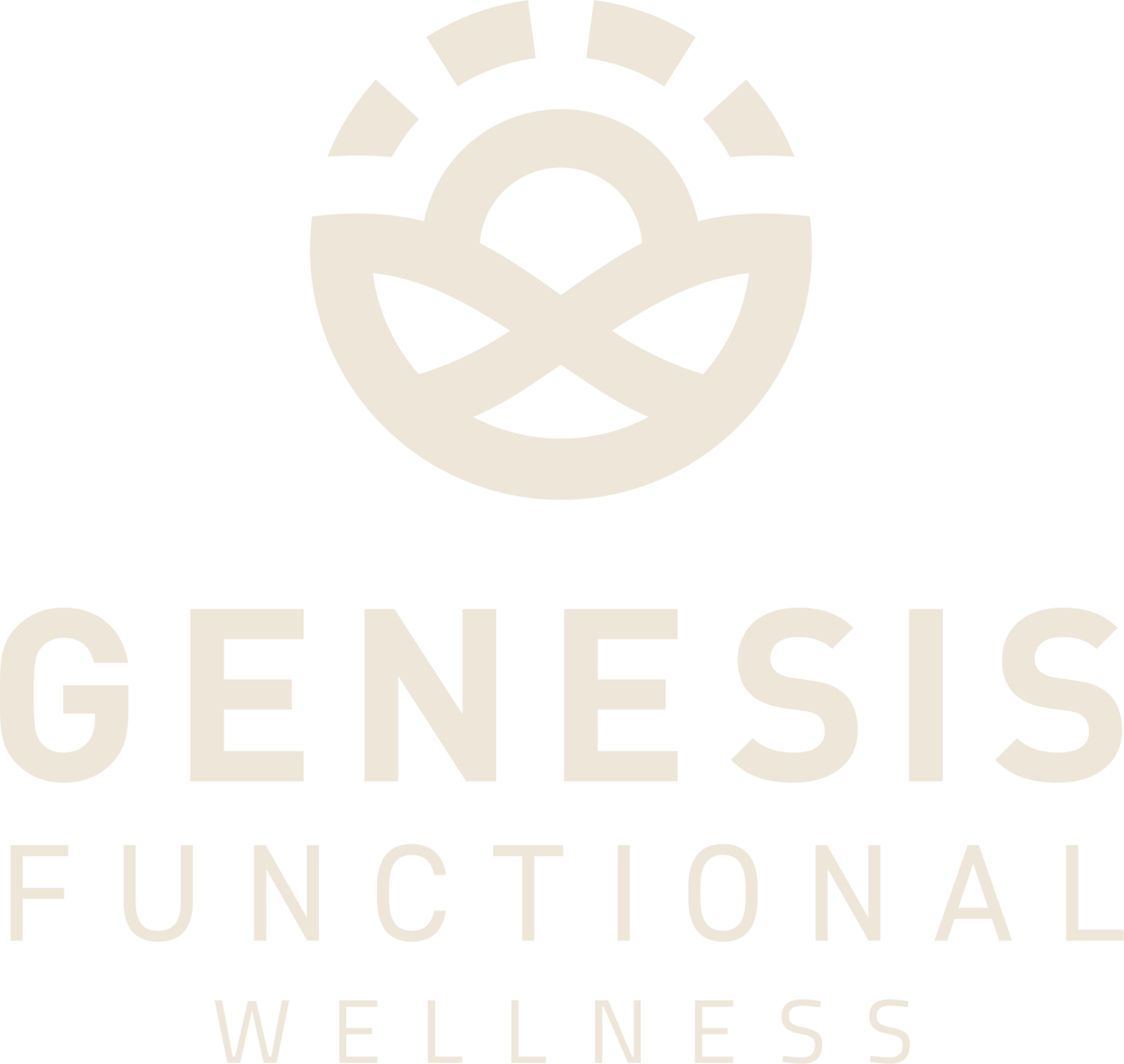
1. Varicoceles and Male infertility
Varicoceles are also referred to as scrotum varicose veins. A varicocele is an enlargement of veins in the scrotum that drain the testicle. This leads to poorly functioning valves, increased testicular temperature, and problems with the synthesis of sperm and testosterone. Having varicoceles leads to reduced sperm count and quality. Oftentimes there are no signs or symptoms of varicoceles, though in some cases, they may cause pain, testicular atrophy, or infertility.
Causes of varicoceles may include:
Lifestyle factors, such as smoking
Oxidative stress
Inability to make or have glutathione (an important our master antioxidant)
Hormonal imbalance
Hyperthermia
Exposure to toxic substances
Testicular blood flow
Venous pressure
Reactive oxygen species or ROS (free radicals)
Genetic factors
Treatments for Varicoceles
Oftentimes, varicoceles don’t require treatment, but in the event of pain, infertility, or testicular atrophy, they may require varicoceles repair procedures. These include:
Open surgery
Microsurgical surgery
Laparoscopic surgery
In addition to varicocele surgical procedures, there are some other options that may help with varicoceles:
Dietary Changes- Processed and inflammatory foods may contribute to varicoceles formation. On the other hand, increasing high-fiber foods like fruits and vegetables may help with the reduction of varicoceles. These foods are able to help with the structural integrity of blood vessels. Additionally, the high fiber may reduce straining during bowel movements, which could theoretically help with scrotal veins.
Supplementing with Glutathione- As varicoceles may be due in part to oxidative stress and a lack of glutathione production, supplementing with glutathione may help reduce oxidative stress and varicoceles.
Kegel Exercises/Pelvic Floor Therapy- Consistent kegel exercises can improve blood flow and muscle tone, which may help with varicoceles.
Varicocele Embolization- This procedure consists of a small catheter that is inserted into the problematic veins. Via the catheter, the radiologist then inserts small metal coils or a solution that causes scarring to block the vein.
2. Retrograde Ejaculation and Male Infertility
When semen enters the bladder during orgasm instead of leaving the penis, this is called retrograde ejaculation. Little or no semen is released in this condition.
Retrograde Ejaculation causes
There are various causes involved when it comes to retrograde ejaculation. These may include:
Bladder surgery
Prostate surgery
Urethra surgery
Spinal injuries
Diabetes
Nerve damage caused by medical illness, such as uncontrolled diabetes or multiple sclerosis
Medications, such as certain medications that treat an enlarged prostate gland, depression, and psychosis.
Treatment Options for Retrograde Ejaculation
Retrograde ejaculation is determined by testing the urine after ejaculating. If a high amount of semen is found in the ejaculate, then a diagnosis of retrograde ejaculation is given. With the exception of infertility, retrograde ejaculation does not cause any major issues to the body. However, in the case of infertility, treatment may be necessary.
If medication is a possible cause, simply switching medications may be an easy fix.
If your cause is a mild nerve or muscle issue with the bladder, then you may be prescribed a drug that improves muscle tone at the bladder entrance (e.g., pseudoephedrine, imipramine)
If retrograde ejaculation is due to severe damage of the bladder nerves or muscles, then you may need to contact a fertility specialist who might recommend intrauterine insemination, in-vitro fertilization, or intracytoplasmic sperm injection.
3. Erectile Dysfunction and Male Infertility
Erectile dysfunction (ED) occurs when a man is unable to attain or keep an erection long enough for sexual intercourse. Men can have this condition periodically or it can be a chronic condition. A variety of causes can contribute to this, including psychological factors, medical factors, and lifestyle factors. Chronic erectile dysfunction results in an inability to have intercourse.
Causes of Erectile Dysfunction
High blood pressure
Type 2 diabetes
Poor vascular health/circulation
Kidney disease
Cancer treatments
Antidepressant medication
Anxiety, depression, or stress
Smoking
Illegal drug use
Obesity
Alcohol consumption in excess
Low testosterone
Treatment of Erectile Dysfunction
Addressing lifestyle factors is extremely important in the treatment of erectile dysfunction. Diet changes, exercise, and lowering stress may all be necessary.
Blood sugar handling has a lot to do with male fertility and testosterone production. Males with blood sugar issues, even minor issues, can have shifts in hormone production allowing them to convert their testosterone to estrogen. These males then become estrogen dominant due to the lack of testosterone production. They don’t necessarily always have a lack of hormone, they just have the production shifted into a more “female-like” pattern. This is common to see in men with blood sugar dysregulation issues like insulin resistance, metabolic syndrome, and diabetes.
Blood flow is another important factor that needs to be addressed in ED. Blood flow issues are often a complication that comes along with diseases like insulin resistance, metabolic syndrome and diabetes. This is largely due fatty deposits in the blood vessels and stiffness in the arteries. This is why hypertension and other circulation issues are commonly found in those with more severe patterns of blood sugar dysregulation. Insulin resistance, metabolic syndrome, and diabetes are commonly found in those with ED and vice versa.
There are quite a few medications for erectile dysfunction. However, caution should be used as dosage, side effects, and effectiveness vary. On top of this, we need to always ask WHY a pathway or process is not working. It’s often our body’s way of telling us that something is WRONG.
Medications that encourage testosterone production may be recommended in men who have erectile dysfunction due to low testosterone. Use of a medication that can help encourage testosterone production can be helpful if other foundational causes have been addressed. Clomiphene citrate is one medication that has been found to increase testosterone production while decreasing estrogen production in males. Testosterone is important hormone in the development of sperm. Low testosterone levels can result in less healthy, viable sperm. Testosterone replacement is a male contraceptive and therefore should never be used in males looking to have children.
4. Ejaculatory Duct Blockage
Ejaculatory duct blockage is the rare obstruction or blockage of one or both ejaculatory ducts found in 1-5% of men struggling with infertility. This type of blockage prevents a man from releasing semen. This condition can cause pelvic pain, infertility, or both.
Causes of Ejaculatory Duct Blockage
The cause of ejaculatory duct blockage may be congenital or acquired. Some men are born with an ejaculatory duct blockage. Others can occur due to infections, trauma, or surgery. Some specific causes are listed below:
Common causes of ejaculatory duct blockage
Congenital: Rarely, some men are born with congenital ejaculatory duct blockages
Mullerian duct cyst: A mullerian duct cyst is formed in the male pelvis and can cause a blockage in the ejaculatory duct.
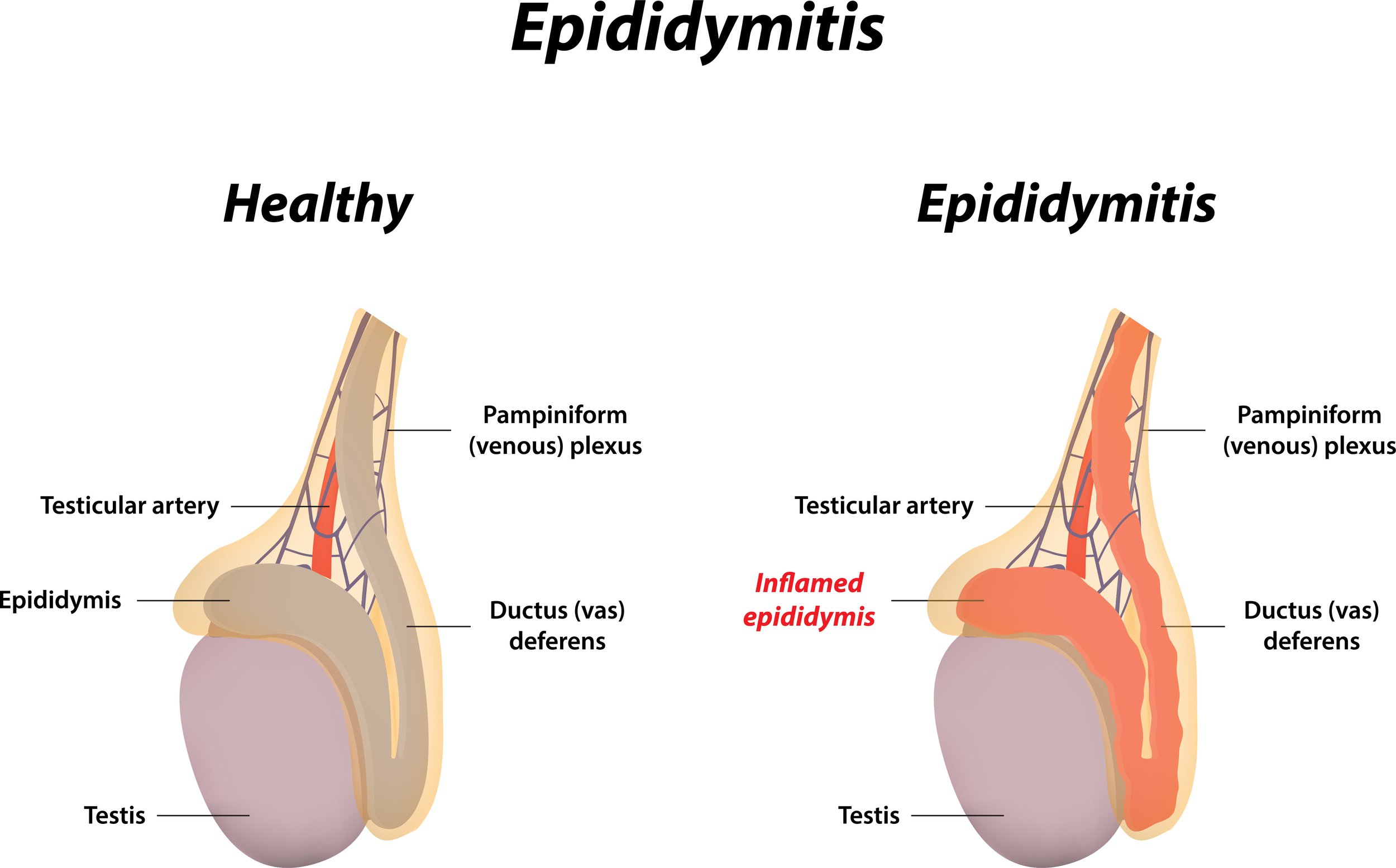
Epididymitis: Epididymitis is the swelling or irritation of the epididymis, which is a coiled tube at the back of the testicles that stores and transports sperm. This can cause intense pain in the testicle region, and it can also cause a blockage in the ejaculatory duct. Epididymitis can be caused by an infection like chlamydia, gonorrhea, or a urinary tract infection.
Surgeries: A vasectomy, can (of course) cause ejaculatory duct blockages.
Treatment of Ejaculatory Duct Blockage
Encouragingly, ejaculatory duct blockages are often treated effectively by transurethral resection of the ejactulatory duct. This procedure is performed endoscopically.
5. Hypospadias
Hypospadias is a penis birth defect. In this condition, the opening of the urethra is on the underside of the penis rather than at the tip. The opening can be anywhere from right underneath the tip of the penis to all the way at the base of the penis, though the latter is not as common.
Causes of Hypospadias
As the penis develops in utero, particular hormones stimulate the development of urethra and foreskin. When the hormones malfunction, the urethra does not develop correctly, which causes the misplaced opening of the urethra. Hypospadias can be genetic, but environment is also thought to play a role, though exact causes are unknown.
Risk Factors for Hypospadias:
Risk factors may include family history, maternal age of over 35, genetic variations, or exposure to certain chemicals when pregnant, though more research is needed to confirm.
Treatment of Hypospadias
Some hypospadias are minor and do not require surgery. More significant hypospadias may need surgery to relocate the opening of the urethra and and sometimes straighten the penis shaft. Surgery is often done when babies are between 6 and 12 months old, but surgery can also be performed on adults.
6. Undescended Testicles
During fetal development, it’s possible that either one or both testicles fail to descend from the abdomen into the scrotum. This condition will make decreased fertility more of a possibility. It also increases the risk of testicular cancer.
Causes of Undescended Testicles
While the causes of undescended testicles are unknown, it’s suspected that a combination of maternal health, genetics, and environmental exposures may contribute to abnormal development.
Treatments for Undescended Testicles
Undescended testicles can be treated through surgery, which can be laparoscopic surgery or open surgery. However, this surgery is recommended before one year of age to reduce risk of infertility or testicular cancer. The earlier the surgery is, the better, but it’s generally recommended that it occurs before a child is 18 months old.
Closing Thoughts
While many of these anatomical issues can appear overwhelming, as you can see, many of these are rectifiable through surgical procedures and/or lifestyle changes. There is absolutely hope! Additionally, there are a variety of other factors that can also contribute to infertility. Our practice specializes in working with couples struggling with infertility. By getting a detailed history, lab work, and imaging we are able to pinpoint root causes for both male and female infertility. Our thorough approach can save couples precious time and money.